Reconstructive Jaw Following Radiation Injury is a critical medical solution for patients who develop severe jaw damage after cancer treatment. Radiation therapy for head and neck cancer can be life-saving, but it sometimes leads to serious long-term effects on the jawbone’s ability to heal. In rare cases, the bone becomes damaged and loses its blood supply, leaving it unable to repair itself. This condition not only threatens oral function but can lead to chronic infection and bone deterioration that significantly affects a person’s quality of life.
When Radiation Damages the Jaw and Reconstructive Jaw Following Radiation Injury Becomes Necessary
Radiation therapy works by destroying cancer cells, but it can also damage normal tissues, including the tiny blood vessels that nourish bone. When blood flow to the jawbone is compromised, the bone can die—a condition that can develop months or even years after treatment. In such cases, reconstructive jaw following radiation injury becomes essential to restore both structure and function.
This situation often presents with exposed bone, recurrent infection, or non-healing wounds in the mouth. Without a reliable blood supply, traditional healing methods such as antibiotics or enhanced oxygen therapy may fail. As a result, progressive weakening of the jawbone occurs, making everyday activities like eating and speaking increasingly difficult.
Advanced Surgical Reconstruction for Reconstructive Jaw Following Radiation Injury
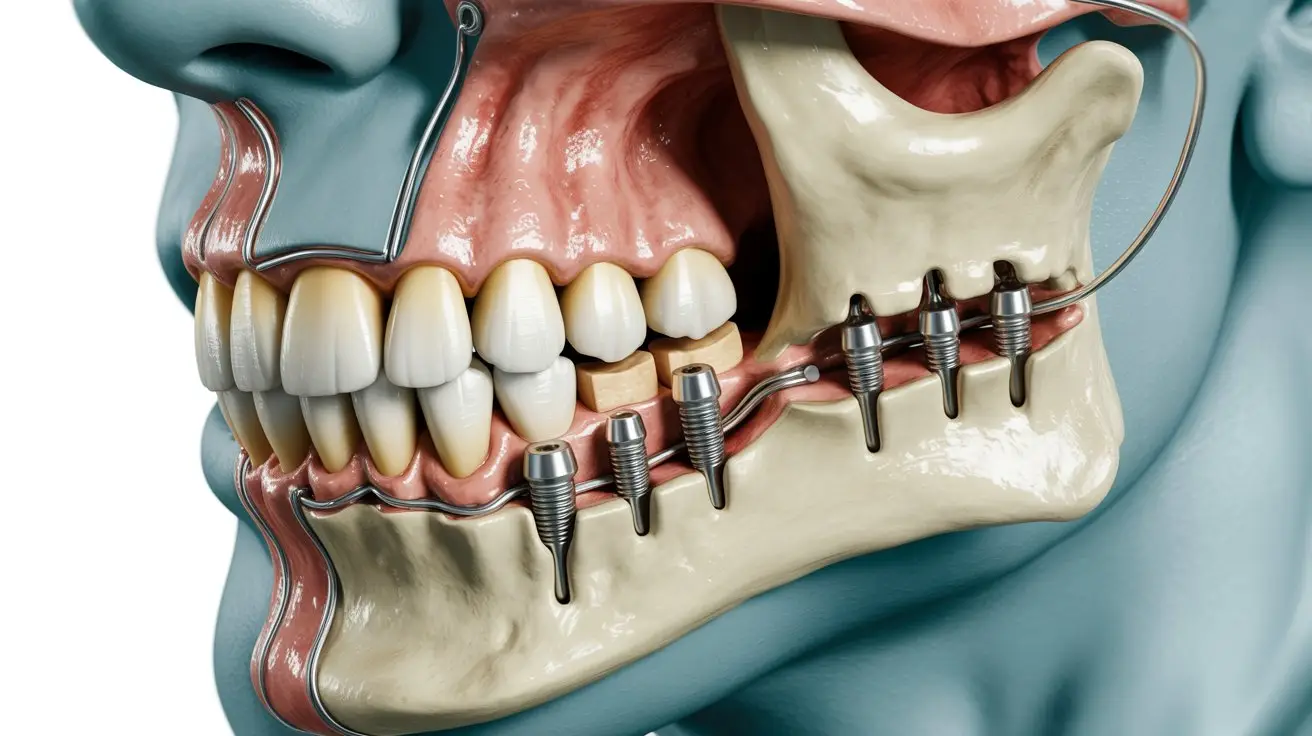
For individuals facing this severe complication, advanced reconstructive surgery offers a way to restore jaw structure and function. The goal of reconstructive jaw following radiation injury surgery is to replace or repair the damaged portion of the jaw with healthy, well-vascularized tissue that can integrate with the surrounding anatomy and support normal jaw movement.
This type of reconstructive procedure is highly specialized and involves several carefully planned stages. Each step is designed to ensure optimal blood supply, long-term stability, and functional recovery of the jaw.
Preparing for Reconstructive Jaw Following Radiation Injury Surgery
A comprehensive evaluation is required before jaw surgery, including advanced imaging studies to assess the extent of bone damage and the amount of remaining healthy tissue. This preparation phase is a cornerstone of successful reconstructive jaw following radiation injury, allowing precise surgical planning and minimizing complications.
Patients may undergo supportive therapies to optimize healing potential prior to reconstruction. This preparatory phase improves surgical outcomes and plays a crucial role in long-term success.
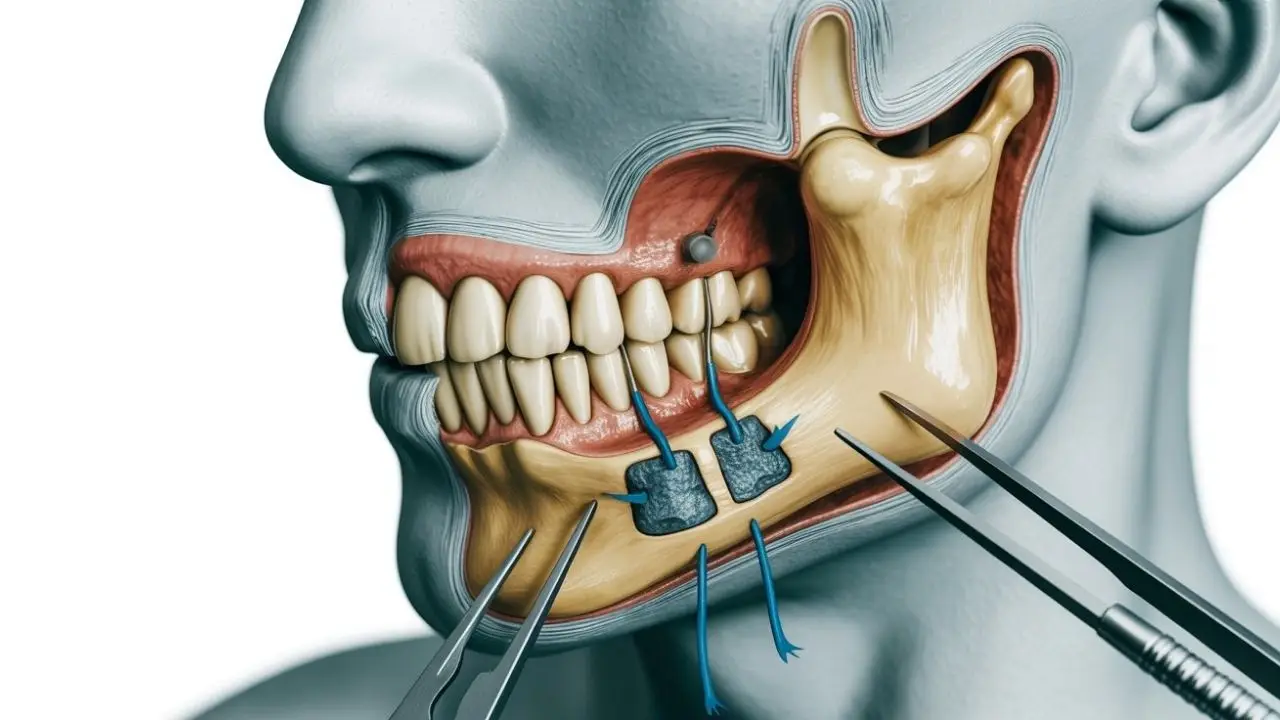
Restoring Blood Supply and Jaw Structure
The cornerstone of reconstructive jaw following radiation injury is restoring blood flow to an area where circulation has been lost. Surgeons remove diseased bone and replace it with transplanted tissue that contains its own blood vessels, allowing the jaw to heal in a way that radiation-damaged bone cannot.
This procedure often uses tissue from another part of the patient’s body to form a new, living foundation for the jaw. The restored blood supply enables both bone and soft tissues to regain normal function and durability.
Hospital Stay and Early Recovery
Although reconstructive jaw surgery is complex, advances in surgical techniques have significantly shortened recovery times. Many patients begin gentle jaw movement shortly after surgery, and hospital stays are often limited to a few days with structured follow-up care.
Early recovery focuses on infection prevention, wound healing, and gradual return of oral function. Patients are often surprised by how quickly they can resume speaking and eating soft foods after reconstructive jaw following radiation injury.
A Transformational Outcome After Reconstructive Jaw Following Radiation Injury
The benefits of successful jaw reconstruction extend far beyond physical repair. Patients who once suffered from chronic pain, infection, and functional loss often regain the ability to eat, speak, and smile comfortably. This transformation significantly improves confidence and overall quality of life.
By restoring both structural integrity and blood supply, reconstructive jaw following radiation injury provides long-term stability and natural healing, making it a truly life-restoring procedure.
The Role of Expert Surgical Care
Managing radiation-related jaw damage requires advanced knowledge of facial anatomy, bone physiology, and microsurgical reconstruction. Prof. Dr. Celal Çandırlı brings extensive experience in reconstructive jaw following radiation injury, combining precision surgery with a patient-centered approach.
Through individualized treatment planning and meticulous execution, patients receive care tailored to their anatomy and health needs, allowing them to overcome complex radiation-induced complications.
Life After Reconstructive Jaw Following Radiation Injury
After reconstruction and healing, patients often experience dramatic improvements in comfort and daily function. Many return to a regular diet, speak more clearly, and engage socially without discomfort or limitation.
Long-term follow-up includes routine dental and surgical evaluations, ensuring the reconstructed jaw remains healthy and functional. With continued care, patients can confidently return to normal life after reconstructive jaw following radiation injury.

Frequently Asked Questions (Reconstructive Jaw Following Radiation Injury)
Radiation therapy can save lives, but its effects on healthy tissues—especially the jaw—can pose lasting challenges. Modern reconstructive jaw following radiation injury techniques now offer reliable solutions for restoring blood supply, strength, and function to the jaw.
With specialized surgical expertise, patients who once had limited options can achieve meaningful recovery and regain the quality of life they deserve.
How Long Does It Take for the Mouth to Heal After Radiation?
Healing of the mouth after radiation therapy varies depending on dose, treatment area, and individual health. Acute side effects such as mouth sores and inflammation often improve within a few weeks after radiation ends. However, full healing of oral tissues and stabilization of salivary function may take several months, and some changes can be long-term.
How Does Radiotherapy Affect the Jaw?
Radiotherapy can damage small blood vessels that supply the jawbone and surrounding tissues. Over time, this reduces oxygen and nutrient delivery, making the bone more fragile and slower to heal. These changes can increase the risk of pain, stiffness, infection, and in severe cases bone necrosis.
Why Can’t You Do Surgery Immediately After Radiation?
Radiation temporarily weakens tissues by reducing blood supply and impairing healing capacity. Performing surgery too soon increases the risk of poor wound healing, infection, and tissue breakdown. Waiting allows tissues to partially recover and improves the safety and success of surgical procedures.
What Is Osteonecrosis of the Jaw After Radiation Therapy?
Osteonecrosis of the jaw is a condition where jawbone tissue dies due to insufficient blood supply following radiation. It can lead to exposed bone, chronic infection, pain, and difficulty chewing or speaking. This condition may develop months or even years after radiation treatment.
Can You Have Reconstructive Surgery After Radiation?
Yes, reconstructive surgery is possible after radiation, but it requires specialized planning. Surgeons often use techniques that bring healthy, well-vascularized tissue into the affected area to support healing. Careful timing and surgical expertise are essential for successful outcomes.
How Long Should You Wait for Surgery After Radiation?
The waiting period depends on the type of surgery and the patient’s condition, but surgeons often recommend waiting several months after radiation. This allows inflammation to subside and tissues to stabilize. In complex cases, surgery may be delayed longer to reduce complications.
What Are the First Signs of Osteonecrosis of the Jaw?
Early signs may include persistent jaw pain, swelling, exposed bone inside the mouth, delayed healing after dental work, or recurrent infections. Some patients also notice numbness or a feeling of heaviness in the jaw. Early detection is critical to prevent progression.
How Does Radiation Impact My Jawbone?
Radiation affects the jawbone by reducing its ability to repair and remodel itself. Bone cells become less active, and blood flow decreases, making the jaw more susceptible to fractures, infection, and delayed healing. These effects can be long-lasting.
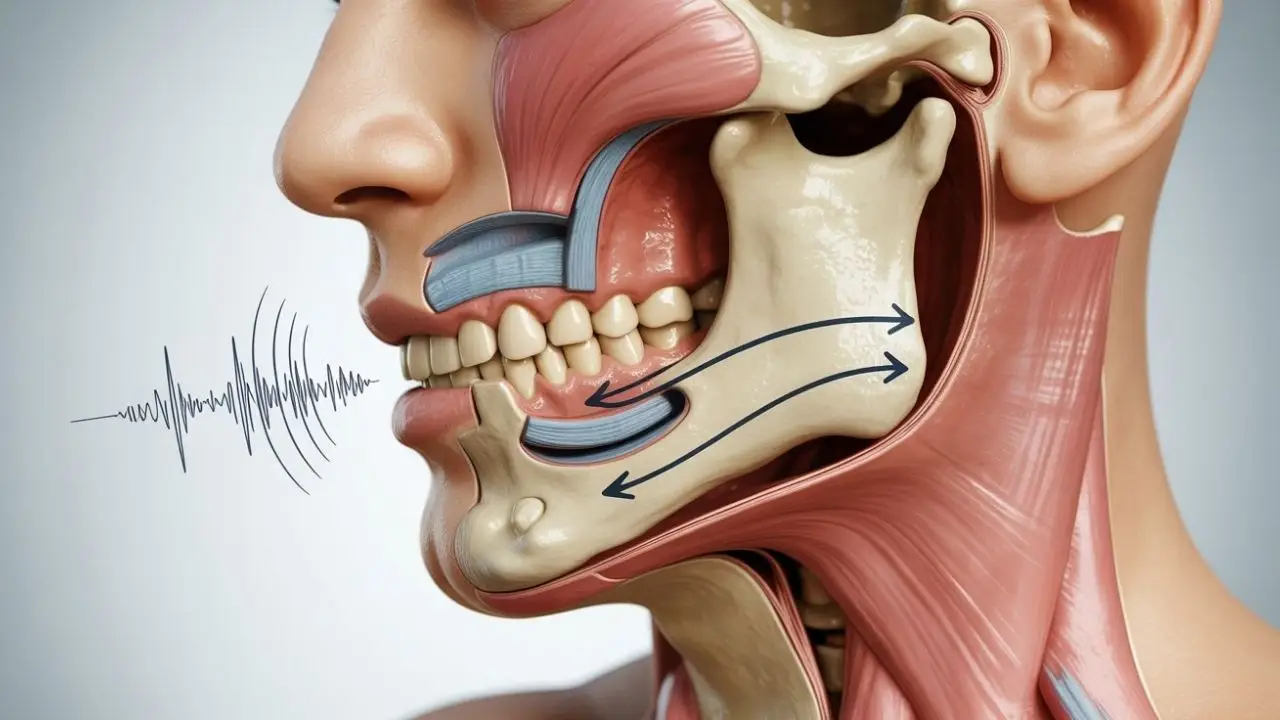
How Do You Treat Trismus After Radiation?
Trismus, or limited mouth opening, is treated with physical therapy, stretching exercises, and jaw-mobilization devices. Early and consistent therapy helps maintain jaw movement and prevent worsening stiffness. In some cases, additional medical or surgical interventions may be required.
Can You Have Dental Work Done After Radiation?
Dental care after radiation is possible but must be approached cautiously. Preventive care and non-invasive treatments are preferred, while extractions or invasive procedures require careful planning to reduce the risk of jaw complications. Coordination between dental and medical teams is important.
When Do Radiation Side Effects Peak?
Most acute radiation side effects peak toward the end of treatment or shortly after it finishes. Symptoms such as mouth sores, pain, and swelling often improve within weeks. Some late effects, however, may appear months or years later.
Why Does My Jaw Hurt After Head and Neck Radiation?
Jaw pain after radiation can result
from inflammation, muscle stiffness, nerve irritation, reduced blood supply to bone, or the development of trismus. Pain may be temporary or persistent depending on the extent of tissue damage. Evaluation is important if pain worsens or does not improve over time.