Temporomandibular Joint Disorders (TMD) are conditions that affect the jaw joint and surrounding muscles, causing pain, clicking, and difficulty with chewing or opening the mouth. In many people, TMD is temporary and improves with simple self-care and non-surgical treatments.
What Is a Temporomandibular Joint Disorder?
Temporomandibular Joint Disorders are problems affecting the temporomandibular joints (TMJ), the muscles that move your jaw, and the surrounding structures. These disorders disrupt the smooth hinge and sliding movements of the jaw, leading to pain, stiffness, joint noises, or locking.
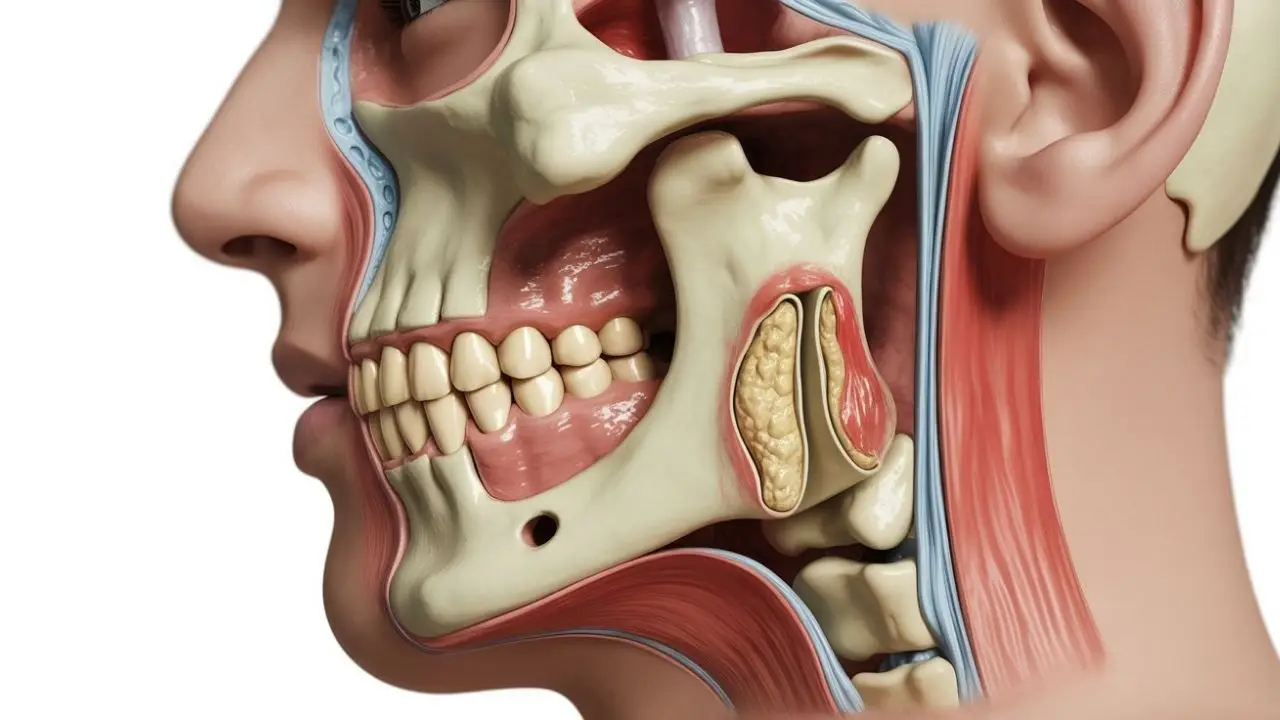
The temporomandibular joints are the two joints that connect your lower jaw (mandible) to the temporal bones of your skull, located just in front of each ear. These joints, together with several muscles and ligaments, allow your jaw to move up and down, side to side, and forward and backward so you can chew, talk, yawn, and swallow comfortably.
Temporomandibular Joint Disorders (TMD) is an umbrella term for conditions that affect:
- The jaw joints themselves.
- The muscles that control jaw movement.
- The ligaments, cartilage disc, and other supporting structures around the TMJ.
When these structures do not work smoothly together, you may develop jaw pain, limited motion, or joint noises such as clicking or popping. In some people, TMD is short-lived; in others, it can become a chronic pain condition.

Types of Temporomandibular Joint Disorders
Experts generally classify Temporomandibular Joint Disorders (TMD) into three main categories. These categories help clinicians understand whether the source of the problem is primarily muscular, mechanical within the joint, or related to degenerative disease. Each type may cause similar symptoms, but the underlying mechanisms and treatment approaches can differ.
Myofascial Pain
Myofascial pain is the most common type of Temporomandibular Joint Disorder. It primarily involves discomfort, tenderness, or tightness in the muscles that control jaw movement and the surrounding connective tissues (fascia). People with myofascial pain often experience aching in the jaw, face, neck, or shoulders, difficulty opening the mouth fully, and headaches related to muscle tension. Stress, clenching, poor posture, and overuse of the jaw muscles frequently contribute to this condition.
Internal Derangement of the Joint
Internal derangement refers to a structural problem within the temporomandibular joint itself. This can include a displaced or damaged cartilage disc, a dislocated jaw, or injury to the bony components of the joint. When the disc is not in its correct position, clicking, popping, or grinding sounds may occur as the jaw moves. In some cases, the jaw may temporarily lock open or closed. Internal derangement can arise after trauma, joint strain, or gradual wear and tear.
Degenerative Joint Disease
Degenerative joint disease includes conditions such as osteoarthritis and rheumatoid arthritis that affect the TMJ. These diseases gradually wear down the cartilage and bone surfaces within the joint, leading to inflammation, stiffness, reduced mobility, and chronic pain. Over time, structural changes may alter how the jaw opens and closes. Management often focuses on reducing inflammation, protecting the joint, and maintaining as much function as possible.
Although these categories are distinct, some people may experience features of more than one type at the same time. A thorough evaluation by a healthcare professional is important to determine the underlying cause and guide appropriate treatment.

Common Symptoms of Temporomandibular Joint Disorders
Symptoms can vary widely from person to person. Some people have only mild discomfort, while others find that TMD significantly affects daily life. Typical symptoms include:
- Pain or tenderness in the jaw, especially near the ears.
- Pain in one or both temporomandibular joints.
- Aching facial pain or pressure around the cheeks and temples.
- Clicking, popping, or grinding sounds when opening or closing the mouth.
- Difficulty chewing or pain while chewing.
- Limited ability to open the mouth fully or a feeling that the jaw is “stuck” or locked.
- Headaches, often around the temples or behind the eyes.
- Neck, shoulder, or upper back pain linked to jaw tension.
- Ear-related symptoms such as earache, fullness, or ringing (tinnitus) without ear infection.
- Changes in the way your upper and lower teeth fit together.
Symptoms may worsen when you chew hard foods, yawn widely, clench your teeth, or are under stress.
When to See a Doctor or Dentist for TMD
Not every jaw click needs treatment. However, you should seek medical or dental advice if you have:
- Ongoing jaw pain or tenderness that does not improve with basic self-care.
- Difficulty opening or closing your mouth fully.
- Jaw locking, particularly if it interferes with eating or speaking.
- Severe or frequent headaches, facial pain, or ear pain associated with jaw movement.
- Jaw pain after injury to the face, head, or neck.
Urgent assessment is especially important if you cannot eat or drink, have rapidly worsening pain, or notice unusual symptoms such as vision changes or severe headache along with jaw pain.

Causes of Temporomandibular Joint Disorders
The exact cause of Temporomandibular Joint Disorders (TMD) is often difficult to identify. In many people, symptoms develop due to a combination of structural problems, muscle tension, habits, and underlying medical conditions. Below are the most common causes and contributing factors, explained in detail.
Jaw Injury or Trauma
An injury to the jaw, face, or neck—such as a direct blow, fracture, or whiplash—can damage the temporomandibular joint and surrounding tissues. Trauma may alter how the jaw moves, trigger inflammation, and increase muscle tension, all of which can lead to persistent pain and dysfunction.
Bruxism (Teeth Grinding and Clenching)
Bruxism refers to grinding or clenching the teeth, often unconsciously during sleep or periods of stress. Continuous clenching places excessive pressure on the jaw joints and surrounding muscles, which can cause pain, stiffness, headaches, and wear on the teeth over time.
Joint Overload and Strain
Habits that overuse the jaw—such as chewing gum frequently, biting nails, holding objects between the teeth, or eating very hard or chewy foods—may overload the TMJ. Repeated strain can irritate the joint and surrounding muscles, eventually leading to Temporomandibular Joint Disorders.
Arthritis Affecting the Jaw Joint
Different forms of arthritis, including osteoarthritis and rheumatoid arthritis, can damage the cartilage, bone, and lining of the TMJ. Degeneration or inflammation inside the joint may result in stiffness, pain, creaking sounds, and reduced range of motion.
Disc Displacement or Damage
A small cartilage disc inside the TMJ helps cushion movement and keeps the joint aligned. If this disc slips out of position, wears down, or becomes damaged, the joint may move irregularly. This can cause clicking or popping sounds, jaw locking, and painful or restricted movement.
Uneven Bite or Jaw Alignment Problems
Structural differences—such as misaligned teeth, jaw asymmetry, or bite problems—may change how the jaw opens and closes. When the bite is imbalanced, the TMJ and muscles must work harder to stabilize movement, which can eventually contribute to pain and dysfunction.
Stress and Muscle Tension
Emotional stress often leads to involuntary habits such as clenching the jaw, grinding the teeth, or tightening facial and neck muscles. Poor posture, particularly from prolonged screen use, may further strain the jaw and cervical muscles, increasing the risk of TMD.
Other Pain and Health Conditions
Some people with Temporomandibular Joint Disorders also have overlapping chronic pain conditions, such as fibromyalgia or chronic fatigue syndrome. These conditions may heighten pain sensitivity and amplify TMD symptoms, making them more persistent.
In many cases, more than one factor is involved. Understanding potential causes helps guide treatment and lifestyle adjustments to protect the jaw joint and reduce long-term discomfort.
Risk Factors for Temporomandibular Joint Disorders
Certain factors may increase the likelihood of developing TMD or make symptoms more persistent:
- Chronic teeth grinding or clenching.
- Existing arthritis or other joint diseases.
- Previous jaw or facial injuries.
- Connective tissue diseases that affect joint support.
- High stress levels, anxiety, or depression.
- Other chronic pain conditions or sleep disturbances.
- Habits such as gum chewing, nail biting, or frequently biting on pens or other objects.
How Are Temporomandibular Joint Disorders Diagnosed?
A healthcare professional (often a dentist, oral and maxillofacial specialist, or physician) will start by taking a detailed medical and dental history and asking about your symptoms, habits, and any injuries or stressors.
During the examination, they may:
- Observe how wide you can open your mouth and whether the movement is smooth or limited.
- Listen and feel for joint noises such as clicking, popping, or grating when you open and close your mouth.
- Press on the jaw joints and facial muscles to check for tenderness or spasm.
- Evaluate how your upper and lower teeth come together (your bite).
If needed, imaging tests may be used to look at the joints, bones, and soft tissues, such as:
- Dental X-rays – to assess the teeth and jaw bones.
- CT scans – to get detailed images of the bony structures.
- MRI – to evaluate the position and condition of the joint disc and surrounding soft tissues.
In some cases, other conditions like tooth decay, sinus problems, ear disease, or nerve disorders can mimic TMD, so your provider may rule these out before confirming the diagnosis.

Surgical and Procedural Treatments for Temporomandibular Joint Disorders
Surgery for Temporomandibular Joint Disorders (TMD) is usually considered only after conservative treatments such as medication, splints, physiotherapy, and lifestyle changes have not provided sufficient relief. It is most appropriate when there is clear structural damage or mechanical dysfunction in the joint. Below are the main surgical and minimally invasive options used to restore function, reduce pain, and improve jaw movement.
Arthrocentesis (Joint Flushing)
Arthrocentesis is a minimally invasive procedure in which sterile fluid is gently flushed through the temporomandibular joint. The goal is to wash out debris, inflammatory byproducts, and scar tissue that may be interfering with smooth joint movement. This process can also help release a “stuck” disc or reduce friction inside the joint.
Because arthrocentesis does not require large incisions, it is often recommended as an early surgical option when patients experience jaw locking, painful clicking, or limited movement that has not improved with conservative treatment. Recovery is typically quicker than with open surgery, and many people notice improvement in both pain and mobility.
Arthroscopy (Keyhole TMJ Surgery)
Arthroscopy is a minimally invasive surgical technique performed using a thin camera (arthroscope) and very small instruments inserted through tiny incisions near the joint. The surgeon can directly view the inside structures of the TMJ on a monitor and perform targeted treatment at the same time.
During arthroscopy, the surgeon may smooth rough joint surfaces, remove inflamed tissue, reposition the cartilage disc, or flush the joint space. This procedure allows for precise repair with less tissue disruption compared to open surgery. Patients generally experience shorter hospital stays, less postoperative pain, and faster return to normal activities, while still benefiting from direct visualization of the joint.
Open-Joint Surgery (Open TMJ Repair or Reconstruction)
Open-joint surgery is the most extensive surgical option and is reserved for severe or complex cases of Temporomandibular Joint Disorders. It may be recommended when there is significant structural damage, bony deformity, severe scarring, tumors, or when the disc or joint surfaces are badly damaged and cannot be managed through arthroscopy or other less invasive techniques.
During open surgery, a larger incision is made near the joint to allow the surgeon full access to the TMJ. Depending on the condition, the procedure may involve disc repair or removal, joint reshaping, scar removal, or even joint replacement in rare and advanced cases. Because this is a major surgery, it carries higher risks and requires longer recovery, so it is generally considered only after other treatment options have failed.
Important: Surgical decisions should always be made in consultation with an experienced TMJ specialist. A thorough evaluation, including imaging and assessment of symptoms, is essential to determine whether surgery is appropriate and which procedure offers the greatest potential benefit with the least risk.
Self-Care Tips for Temporomandibular Joint Disorders
Many people can reduce their TMD symptoms with simple lifestyle and self-care strategies:
- Choose softer foods such as yogurt, eggs, pasta, soups, or stews during painful episodes.
- Avoid hard, crunchy, or chewy foods (like nuts, crusty bread, or chewing gum).
- Try to cut food into smaller pieces to limit jaw strain.
- Practice good posture, especially when working at a desk or using screens.
- Use hot or cold packs (wrapped in a cloth) on the jaw for short periods, depending on what feels better.
- Gently massage tense jaw muscles if advised by your provider.
- Notice and interrupt clenching – your teeth should be slightly apart when you are not chewing.
- Work on stress-reduction techniques such as deep breathing, stretching, mindfulness, or relaxation exercises.
Complications and Outlook
Untreated or severe Temporomandibular Joint Disorders can sometimes lead to long-lasting jaw pain, difficulty chewing a normal diet, disturbed sleep, and wear on the teeth from grinding. However, many people experience gradual improvement with education, self-care, and conservative treatments. Only a small number require invasive procedures.
Early recognition of symptoms, avoiding harmful habits, and seeking professional advice when needed can improve your long-term outlook and help you maintain comfortable jaw function.
Frequently Asked Questions About Temporomandibular Joint Disorders
Are Temporomandibular Joint Disorders serious?
Most cases of Temporomandibular Joint Disorders are not dangerous or life-threatening, and symptoms often improve with time and conservative care. However, severe or persistent pain, jaw locking, or difficulty eating should always be assessed by a healthcare professional to rule out other problems and prevent long-term complications.
Can Temporomandibular Joint Disorders go away on their own?
Yes, TMD symptoms often come and go, and many people notice improvement without formal treatment, especially if they avoid jaw overuse and manage stress. Self-care strategies like eating softer foods, using heat or cold packs, and avoiding clenching can help symptoms settle more quickly.
Do I need imaging tests for TMJ pain?
Not everyone with TMJ pain needs imaging. Your dentist or doctor will first assess your symptoms and examine your jaw. If there are signs of structural damage, persistent unexplained pain, or limited movement, they may order X-rays, CT scans, or MRI to get a clearer picture of the joint and surrounding tissues.
Can Temporomandibular Joint Disorders cause headaches or ear pain?
Yes. TMD can cause pain that spreads to the temples, behind the eyes, into the ears, and down into the neck and shoulders. Some people describe earache, fullness in the ear, or ringing (tinnitus) without any ear infection. Because these symptoms can overlap with other conditions, a proper evaluation is important.
What is the best treatment for Temporomandibular Joint Disorders?
There is no single “best” treatment for everyone. Most people benefit from a combination of self-care, behavior changes, medication for short-term pain relief, and possibly a custom mouth guard. Physical therapy and stress-management techniques are often helpful. Surgery is reserved for selected cases where significant joint damage or persistent symptoms remain despite conservative care.




