TMJ disorders (Temporomandibular joint ), also known as temporomandibular disorders (TMD), affect the joints, muscles, and surrounding tissues that control jaw movement. These conditions can cause pain, functional limitations, and reduced quality of life. Understanding TMJ disorders, their symptoms, and underlying causes is the first step toward effective management and treatment.
What Are Temporomandibular Disorders (TMD)?
Temporomandibular disorders refer to a group of conditions that affect the temporomandibular joint, the muscles responsible for jaw movement, or both. The TMJ connects the lower jaw (mandible) to the skull and plays a crucial role in speaking, chewing, yawning, and facial expressions.
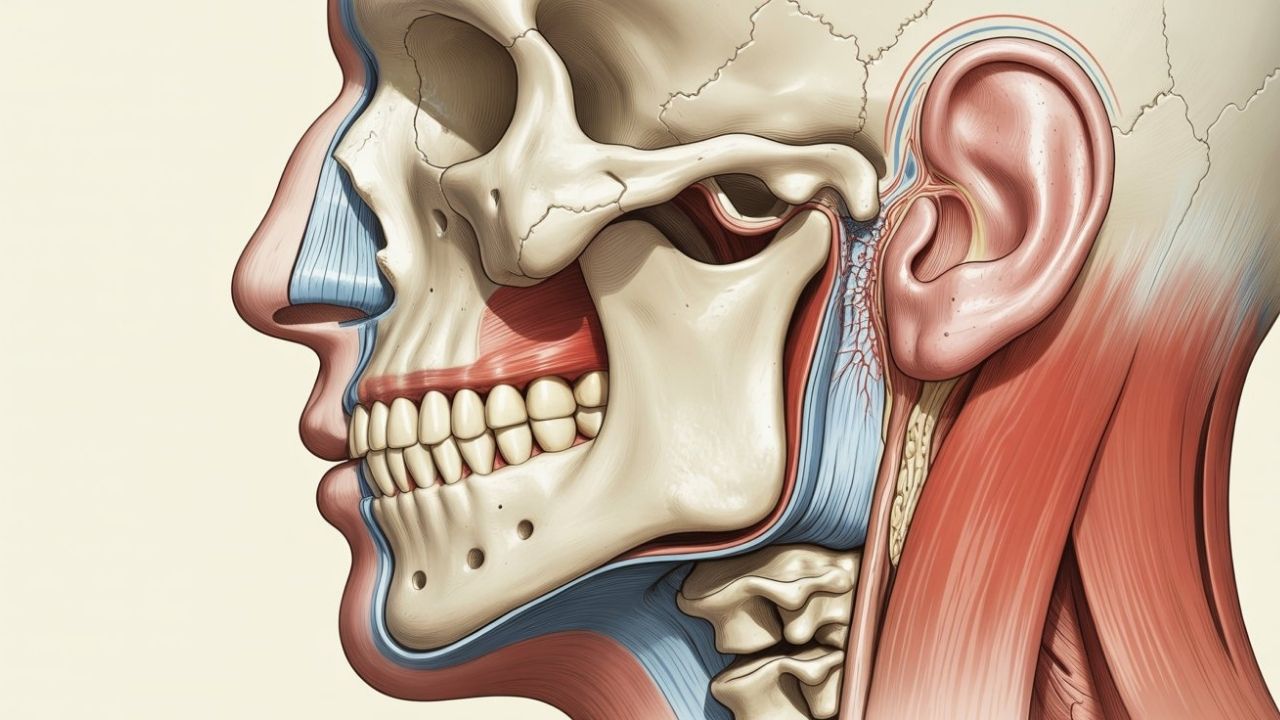
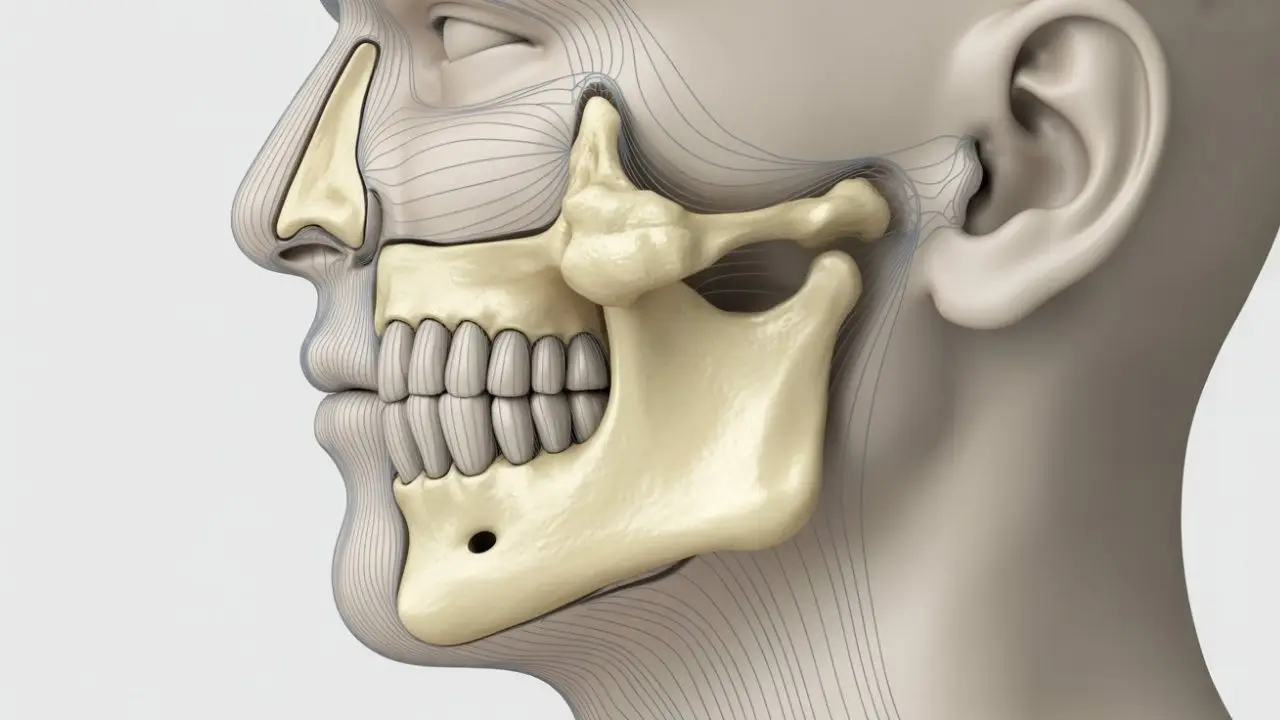
Understanding the Temporomandibular Joint
The temporomandibular joint is one of the most complex joints in the human body. It allows both hinge-like and sliding movements, enabling the jaw to move up and down, side to side, and forward. Because of this complexity, the joint is vulnerable to stress, injury, and muscular imbalance.
TMJ vs. TMD: What’s the Difference?
TMJ refers to the anatomical joint itself, while TMD describes disorders that cause pain or dysfunction in the joint, muscles, or surrounding structures. In everyday language, the terms are often used interchangeably, but medically, TMD is the correct term for the condition.

Common Symptoms of TMJ Disorders
TMJ disorder symptoms can vary from mild discomfort to severe, chronic pain. Symptoms may appear gradually or suddenly and can affect one or both sides of the jaw.
Pain-Related Symptoms
Pain is the most common symptom of TMJ disorders. Individuals may experience jaw pain, facial tenderness, or aching around the ears. The pain can spread to the neck, shoulders, or temples and may worsen with jaw movement or stress.
Jaw Movement and Functional Problems
Many people with TMJ disorders notice difficulty when opening or closing the mouth. Jaw stiffness, locking, or limited range of motion are common. Clicking, popping, or grinding sounds during jaw movement may also occur, with or without pain.
Additional Symptoms
TMJ disorders may also cause headaches, ear fullness, ringing in the ears (tinnitus), dizziness, or tooth sensitivity. Because these symptoms overlap with other conditions, TMJ disorders are sometimes misdiagnosed.
What Causes TMJ Disorders?
There is no single cause of TMJ disorders. In most cases, symptoms result from a combination of physical, behavioral, and psychological factors.
Physical and Structural Causes
Common physical causes include jaw injuries, trauma to the face or neck, arthritis affecting the joint, or displacement of the cartilage disc within the joint. Bite misalignment and missing teeth may also contribute to uneven jaw pressure.
Muscle Tension and Habits
Teeth grinding or clenching (bruxism) places excessive stress on the jaw muscles and joints. Repetitive habits such as chewing gum, nail biting, or poor posture can also overload the temporomandibular joint over time.
Stress and Psychological Factors
Stress plays a significant role in many TMJ disorders. Emotional stress can increase muscle tension, jaw clenching, and pain sensitivity, making symptoms more severe or persistent.

How TMJ Disorders Are Diagnosed?
Diagnosis typically begins with a detailed medical and dental history, followed by a physical examination of the jaw. A healthcare professional may assess jaw movement, muscle tenderness, joint sounds, and pain patterns.
Imaging and Additional Tests
In some cases, imaging such as X-rays, MRI, or CT scans may be used to evaluate the joint structure, cartilage disc position, or surrounding tissues. These tests help rule out other conditions and guide treatment planning.
Treatment and Management Options for TMJ Disorders
Most TMJ disorders can be managed with conservative, non-surgical treatments. The goal is to reduce pain, improve function, and prevent symptom progression.
Self-Care and Lifestyle Adjustments
Initial treatment often includes eating soft foods, avoiding excessive jaw movement, applying heat or cold packs, and practicing stress management techniques. These measures can significantly reduce symptoms for many patients.
Therapeutic and Medical Treatments
Physical therapy, jaw exercises, oral splints, and medications such as pain relievers or muscle relaxants may be recommended. In rare cases where conservative treatments fail, advanced interventions may be considered.
When to See a Specialist
If jaw pain persists, worsens, or interferes with daily activities such as eating or speaking, evaluation by a qualified healthcare professional is recommended. Early diagnosis and appropriate management can help prevent long-term complications.
Frequently Asked Questions (TMJ Disorders)
TMJ disorders are common but often manageable conditions. By recognizing symptoms early and understanding potential causes, individuals can take proactive steps toward relief. With proper evaluation and personalized treatment, most people with TMJ disorders experience significant improvement in their symptoms and quality of life.
What is the most common TMJ disorder?
The most common TMJ disorder is myofascial pain disorder, which affects the muscles that control jaw movement rather than the joint itself. It is often linked to muscle overuse, stress-related clenching, or teeth grinding and typically causes facial pain, jaw soreness, and headaches.
What is the best treatment for TMJ?
There is no single “best” treatment for TMJ disorders, as management depends on the cause and severity of symptoms. In most cases, conservative treatments such as self-care, physical therapy, stress management, and oral splints are effective. Surgery is rarely needed and is considered only when other treatments fail.
How to fix TMJ naturally?
Natural TMJ management focuses on reducing jaw strain and muscle tension. Common approaches include eating soft foods, avoiding excessive jaw movements, applying warm or cold compresses, practicing relaxation techniques, improving posture, and performing gentle jaw exercises. These methods can significantly reduce symptoms in mild to moderate cases.
Is TMJ a permanent condition?
TMJ disorders are not usually permanent. Many people experience temporary symptoms that improve with conservative treatment and lifestyle changes. However, if left untreated or caused by chronic factors such as arthritis or severe bruxism, symptoms may persist or recur over time.
What is the 3 finger test for TMJ?
The three finger test is a simple way to assess jaw mobility. A person attempts to place three fingers stacked vertically between their upper and lower front teeth. Difficulty doing so may indicate limited jaw opening, which can be a sign of TMJ dysfunction.
What is Stage 4 TMJ disorder?
Stage 4 TMJ disorder refers to advanced joint degeneration, often associated with osteoarthritis of the temporomandibular joint. At this stage, the cartilage may be severely worn, bone changes can occur, and symptoms may include chronic pain, significant jaw stiffness, and reduced joint function.
What vitamin deficiency causes TMJ?
There is no single vitamin deficiency that directly causes TMJ disorders. However, deficiencies in vitamin D, magnesium, or B vitamins may contribute to muscle pain, inflammation, or nerve sensitivity, which can worsen TMJ symptoms in some individuals.
What is the best sleeping position for TMJ?
The best sleeping position for TMJ is generally on the back with proper neck support. This position helps keep the jaw and spine aligned and reduces pressure on the temporomandibular joint. Sleeping on the stomach or resting the jaw on the hand may worsen symptoms.
Can a dentist fix TMJ?
A dentist can play an important role in diagnosing and managing TMJ disorders. Dentists may provide oral appliances, evaluate bite alignment, and help manage teeth grinding. In complex cases, treatment may involve collaboration with specialists such as oral and maxillofacial surgeons or physical therapists.
What is the root cause of TMJ?
TMJ disorders usually result from a combination of factors rather than a single root cause. Common contributors include jaw injury, muscle overuse, teeth grinding, arthritis, stress, and poor posture. Identifying individual triggers is essential for effective treatment.
What is the newest treatment for TMJ?
Newer approaches to TMJ management focus on minimally invasive and regenerative techniques. These may include advanced physical therapy protocols, ultrasound-guided injections, platelet-rich plasma (PRP) therapy, and improved oral appliance designs. Research is ongoing, and availability may vary.
What should I avoid if I have TMJ?
If you have TMJ, it is recommended to avoid hard or chewy foods, gum chewing, wide yawning, nail biting, teeth clenching, and poor posture. Reducing stress and avoiding habits that strain the jaw can help prevent symptom flare-ups.